Eye Surgery FAQ’s
What is presbyopia?
Presbyopia is the condition in which the lens of the eye loses its ability to focus. It is a common condition that could accompany cataracts and impair your ability to see objects that are close up. Have you ever found yourself holding a menu or book farther away to read it? the need for reading glasses is usually a sign of presbyopia. This aging of the eyes eventually affects everyone. If you have cataracts with presbyopia, the lens can correct both conditions.
What is a multifocal lens?
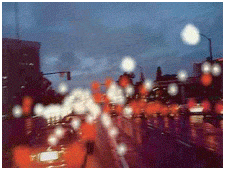
Multifocal lens is a breakthrough lens for cataract surgery that lets patient see from near to far, usually without glasses. It is effective when placed in both eyes. Most of the multifocal lens patients find that they can read a book, work on the computer, drive a car – day or night – and play golf or tennis with an increased freedom from glasses. You my experience visual disturbances in low lighting conditions, therefore increased care should be taken when driving at night
|
|
| Normal Vision | Vision with Cataract(simulated) |
Cataract
Besides conventional extracapsular cataract extraction,this centre is also performing world class small incision sutureless cataract surgery (phaco),with foldable IOL including multi focal leading to greater patient satisfaction.well experienced and highly skilled cataract surgeons of this hospital have changed the lives of thousands of patients who underwent cataract surgery in this centre
A cataract occurs when the normally clear lens of the eye becomes cloudy and interferes with light passing through the eye. Cataracts are a process of aging and usually begin developing around midlife. Approximately 70% of people over the age of 60 and 90% of people over 70 will develop cataracts. The process is generally gradual, and people often do not realize what is happening until they have an eye exam. Common symptoms of cataracts may include blurry vision, glare and reduced vision in bright light, halos around light, poor night vision or fading of colors. Untreated, cataracts are a common cause of blindness.
How is a Cataract Removed?
Modern surgical techniques have made cataract removal one of the safest and most successful surgeries today. The virtually painless procedure takes about 10 minutes and is usually performed in a hospital on an outpatient basis. The eye is anesthetized using eyedrops, and a small incision (about one-eighth of an inch) is made in the white of the eye or through the outer edge of the cornea. An ultrasonic instrument is inserted and used to emulsify, or break up, the cataract and then vacuum away the damaged material. After the cataract has been removed, the surgeon inserts an intraocular lens to replace the natural lens that was removed. The day after surgery you will return for a checkup and your doctor may ask you to return later for one or more follow-up examinations and vision tests. Most patients notice an improvement in their vision during the first few days after surgery.

What is an Intraocular Lens?

An intraocular lens (IOL) is usually implanted during cataract surgery to replace the clouded natural lens that is being removed. A comprehensive eye examination prior to surgery and discussion with your doctor will determine what type, size and power of IOL is needed. The prescription lens implants are made from a flexible plastic that can be folded and inserted into the same small incision used to remove the cataract. The IOL is held in place inside the eye by tiny wires attached to the implant. Once the lens is implanted, it functions similarly to a natural lens and usually is not detectable to the patient.
A cataract occurs when the normally clear lens of the eye becomes cloudy and interferes with light passing through the eye. Cataracts are a process of aging and usually begin developing around midlife. Approximately 70% of people over the age of 60 and 90% of people over 70 will develop cataracts. The process is generally gradual, and people often do not realize what is happening until they have an eye exam. Common symptoms of cataracts may include blurry vision, glare and reduced vision in bright light, halos around light, poor night vision or fading of colors. Untreated, cataracts are a common cause of blindness.
Cataract & Astigmatism
What is Astigmatism?
Sometimes the surface of the cornea is curved in such a way that vision becomes distorted or blurred. A person who has both cataracts and a corneal astigmatism will not regain high – quality distance vision after cataract surgery unless the astigmatism is also corrected.
How does TORIC IOL give better result in cataract surgery?
The toric intraocular lens (IOL) replaces your eye’s natural clouded lens during cataract surger. It has the ability to reduce or eliminate corneal astigmatism at the same time it corrects cataracts. The result is typically improved distance vision and less dependence on spectacles . however , most patients still need corrective lenses for near and intermediate tasks. With the toric lens, your distance vision can be clear and vibrant, giving you the power to see your best and be your best.
 |
 |
 |
| Vision with Cataract | traditional replacement | Vision with Toric IOL |
Proliferative diabetic retinopathy(PDR)
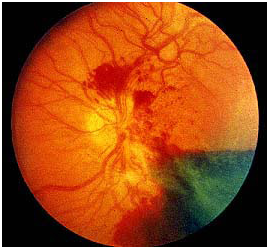
Diabetic eye disease is a leading cause for blindness registration among working age adults in India. It is caused by changes to the tiny blood vessels of the retina (the light sensitive layer at the back of the eye). Proliferative diabetic retinopathy is caused by abnormal new blood vessels that grow on the surface of the retina. This is the most advanced stage of diabetic retinopathy. At this stage, you may not have symptoms but are at high risk for vision loss.
How does proliferative diabetic retinopathy cause vision loss?
In proliferative diabetic retinopathy, the blood vessels that nourish the retina are blocked. The retina sends signals that trigger the growth of new abnormal blood vessels. These vessels are thin and fragile. By themselves, they do not cause vision loss. However, vision loss occurs when they bleed into the retina and gel-like fluid fills the eye.
In advanced stages of proliferative diabetic retinopathy, scar tissue pulls the retina away from the back of the eye (retinal detachment). Abnormal blood vessels can also increase the pressure within the eye (rubeotic glaucoma). If left untreated,severe vision loss and even blindness will occur.
Who is at risk of proliferative diabetic retinopathy?
All people with type 1 and type 2 diabetes are at risk of proliferative diabetic retinopathy. The longer you have had diabetes, the more likely you are to develop this condition. However, large studies have shown that the people who have good control of their blood sugar levels, cholesterol, and blood pressure are less likely to develop proliferative diabetic retinopathy.
How is proliferative diabetic retinopathyfound?
Proliferative diabetic retinopathycan be found during your yearly visit to your ophthalmologist.You may not notice
any changes in your vision at this stage but digital photographs of your eye may show signs of proliferative diabetic retinopathy.It is important you carry on going to your regular diabetic eye screening appointments.
What happens when I go to the medical retina clinic?
You will have a comprehensive eye examination that includes:
- Visual acuity test: A sight test that measures how well you see at different distances
- Eye pressure test: We check the pressure of your eyes. Numbing drops may be used as part of this test.
- Dilated eye examination: Drops are place in your eyes to widen (dilate) your pupils so that we can examine the back of your eyes.You may also undergotests such as:
- Optical coherence tomography (OCT): This test is similar to having a photograph taken of your eye. Pictures are taken using light reflected from the back of your eye. This test allows the eye care practitioner to identify fluid collecting in the macula and plan your treatment.
- Widefield retinal photography: This test is also similar to having a photograph taken of your eye. It takes only a few seconds to take a wide-angled image of the retina. This test allows the eye care practitioner to assess and monitor the severity of diabetes in your eye.
- Fluorescein angiography: In this test, dye is injected into a vein in your arm. Pictures are taken as the dye passes through blood vessels in theeye. This test allows the eye care practitioner to identify leaking blood vessels in the eye and plan your treatment.
How isproliferative diabetic retinopathy treated?
Proliferative diabetic retinopathy is treated with laser therapy. This is done together with improving thecontrol of your blood sugar, blood pressure, and cholesterol levels.
If you have very advanced proliferative diabetic retinopathy, you may require surgery.The treatments for proliferative diabetic retinopathy are:
- lasertherapy
- surgery
What is laser therapy?
This treatment uses laser to produce small areas of heat on the retina. This creates small laser burns scattered across the retina. Usually a thousand laser burns are applied in one session. Usually two to three sessions will be required to achieve this.The goal of laser therapy is to cause the abnormal blood vessels to shrink and disappear.
Laser therapy does not improve your vision. The aim is to prevent severe vision loss.
What happens duringlaser therapy?
Laser therapy takes place in the outpatient medical retina clinic. You will have drops to widen your pupils and numb your eye. The lights in the room will be dim. You will sit facing the laser machine and the doctor will place a contact lens on your eye. This will allow the doctor to see to the back of the eye and prevent you from blinking. During laser therapy, you will see flashes of light. You may feel a stinging sensation that can be uncomfortable. After laser therapy, your vision will be a little blurry for the rest of the day. You will need someone to accompany you home after the treatment. You may wish to bring a pair of sunglasses as your eyes will be sensitive to bright lights.
What are the side effects of laser therapy?
You may experience temporary worsening of vision on the day of laser therapy. This is caused by the bright flashing lights from laser treatment. This usually recovers by the next day. There is a small risk of loss of side vision (visual field) because of laser therapy. More than 90% of persons who receive laser will retain enough side vision for driving. In proliferative diabetic retinopathy, the risk of vision loss from no treatment is much higher than laser therapy. Sometimes laser therapy does not workand yourvision can still get worse despite treatment.
Can I drive after laser therapy?
The driver and vehicle licensing authority makes the decision on whether you will be able to drive. You should inform the Licensing authority when you have had laser therapy. They will arrange to have your side vision (visual field) tested at your local optometrist before making a decision.
What is retinal surgery for proliferative diabetic retinopathy?
In proliferative diabeticretinopathy, bleeding can occur in the retina and gel-like fluid that fills the eye. This blood usually clears on its own within three to six months. If this fails to clear you may need surgery to remove the blood. In advancedproliferative diabetic retinopathy,scar tissue can form in the retina. This causes the retina to pull away from the back of the eye (retinal detachment). Surgery will be required to remove the scar tissue and repair the retina.
Infective conjunctivitis
What is conjunctivitis?
The surface membrane of your eye is known as the conjunctiva. It forms a thin transparent layer over the white of your eye and under your eyelids. Conjunctivitis means inflammation of the conjunctiva. It has several causes:
- An infection (bacteria or viruses, usually flu or cold viruses)-infective conjunctivitis.
- An allergy-allergic conjunctivitis.
What are the symptoms of infective conjunctivitis?
Infective conjunctivitis can affect one eye or both eyes. The whites of your eyes can look inflamed, swollen and red. Your eyes may feel gritty, watery or sticky and your eyelids may become swollen and get stuck together, especially in the mornings. Your vision may be blurred due to tears or sticky discharge. You may also get flu-like symptoms such as a sore throat, fever, muscle ache, and feel generally unwell.
What are the treatment options for infective conjunctivitis?
- No treatment–most infections clear up on their own within a few days to a few weeks.
- Antibiotic eye drops or ointment–viral infections do not respond to antibiotics and the infection may last for two to three weeks before your natural immunity is able to build up enough to clear the virus. Antibiotic drops or ointment may be helpful in conjunctivitis caused by bacteria.
- Lubricant eye drops, gel or ointment–these may help reduce discomfort and grittiness, but will not reduce the duration of the illness.
- Simple painkillers such as paracetamol or ibuprofen tablets can ease the discomfort and flu-like symptoms.
- Regular lid cleaning–you can clean sticky discharge or secretions from your eyes with a clean flannel soaked in warm water.
- Steroid eye drops are occasionally used in severe cases.
What is the infection risk to others?
Viral conjunctivitis is contagious and spreads very easily through water droplets (coughs and sneezes) or contact with tissues, flannels, towels, pillowcases and even door handles. They can also be caught through droplets spread by sneezing and coughing. Not sharing towels/pillows and encouraging your child to wash their hands often is important to reduce the spread.
Frequent hand-washing and proper disposal of used tissues is important in preventing the spread of the condition to other family members or work colleagues.
Advice for contact lens wear. Contact lenses should not be worn until symptoms have completely cleared.
Are there any complications?
Occasionally, viral conjunctivitis can cause inflammation on the cornea, the front window of the eye, or scarring of the conjunctiva, which can affect the sight, however this usually responds well to treatment.
When to seek advice?
If you develop further blurred vision or noticeable eye pain, or if you see any blisters or spots on your eyelids, you should call for advice.
Diabetic macular oedema
What is diabetic macular oedema?
Diabetic eye disease is a leading cause of blindness registration among working age adults in India. It is caused by changes to the tiny blood vessels of the retina (the light sensitive layer at the back of the eye). In diabetic macular oedema, blood vessels leak fluid into the retina.
How does diabetic macular oedema cause vision loss?
Vision loss occurs when the fluid reaches the macula (the centre of the retina that provides sharp vision) and builds up, causing swelling. At first, you may not notice changes to your vision. Over time, diabetic macular oedema can cause your central vision to become blurred. A healthy macula is essential for good vision.
Who is at risk of diabetic macular oedema?All people with type 1 and type 2 diabetes are at risk of diabetic macular oedema. You are at greater risk if you:
- Have had diabetes for a long time–about one in three people living with diabetes for 20 years or more will develop diabetic macular oedema
- Have poorly controlled blood sugars
- Havehigh blood pressure
- Have high cholesterol levels
- Smoking
- Pregnancy
- Visual acuity test: A sight test that measures how well you see at different distances
- Eye pressure test: A test that measures the pressure of your eyes –numbing drops may be used as part of this test
- Dilated eye examination: Drops are placed in your eyes to dilate (widen) your pupils so that the back of your eyes can be examined You may also undergo tests such as a:
- Fluorescein angiography, a diagnostic test which involves the injection of fluorescein (yellow) dye into your bloodstream via a vein in your hand or arm, followed by a series of retinal photographs taken over several minutes. The test gives your doctor more information about the condition of your retina and this helps decide which treatment is most appropriate.
- Optical coherence tomography (OCT) measures the amount of retinal swelling (macular oedema) which, like fluorescein angiography, helps decide which treatment is most appropriate. OCT is also used to monitor your retina over time and to show how effective treatment may have been. It is effectively ‘optical ultrasound’, a non-invasive test, using reflections from within your retina to provide a cross-sectional picture of the retina.
Large studies have shown that people who have well-controlled blood sugar, blood pressure and cholesterol levels, and do not smoke are less likely to develop diabetic macular oedema.
How to reduce the risks of diabetic macula oedema?
To reduce the risk of diabetic macular oedema, it is important not to smoke and to ensure that your blood sugar, blood pressure, and cholesterol levels are well controlled.
How is diabetic macular oedema detected?
Diabetic macula oedema may be detected during your annual eye screening visits, which are offered to all patients with diabetes. Digital photographs of your retina may show signs of early diabetic macular oedema. You may not notice any changes in your vision at this stage. If diabetic macular oedema is detected, you will be referred to the retina clinic.
What happens when I attend the medical retina clinic? You will have a comprehensive eye examination that includes:
Anti- VEGF intravitreal injection treatment
This leaflet is written for patients who might have treatment with anti-angiogenic (anti-VEGF) drugs via an injection into the eye. This treats certain retinal conditions which cause abnormal blood vessels to grow and leak under the retina.
Patients with these retinal conditions can lose central vision when abnormal blood vessels bleed or leak fluid under the retina at the back of the eye. A series of injections of anti-VEGF medicines are given into the back of the eye to stop these blood vessels growing and help control the leakage. This treatment is highly effective in preserving central vision in many people.
In which common conditions might this occur?
- Wet age-related macular degeneration.
- Myopic choroidal neovascularization.
- Diabetic macular oedema.
- Retinal vein occlusion.
- Any other retinal condition causing fluid to leak under the retina.
What is age-related macular degeneration (AMD)?
Age-related macular degeneration (AMD) is the leading cause of vision loss in people aged 50 years or older. It involves damage to the part of the eye called the macula. The macula is a small, but extremely important area located at the centre of the retina, the light-sensing tissue that lines the back of the eye.
Sub-retinal bleeding at the macula in wetmacular degenerationThe macula is responsible for seeing fine details clearly. A person with AMD loses the ability to see fine details, both close-up and at a distance. This affects only the central vision, with the side, or peripheral, vision usually remaining normal. For example, when people with AMD look at a clock, they can see the clock’s outline but cannot tell what time it is. In a similar way, those with AMD will also lose the ability to recognise people.
What is ‘wet’ AMD?
There are two types of AMD. Most people (about 75%) have a form called ‘early’ or ‘dry’ AMD, which develops when there is a waste build-up under the macula. This is usually seen in those with normal or partially reduced vision. A minority of patients with early AMD can progress to the vision-threatening forms of AMD called late AMD. The most common form of late AMD is ‘exudative’ or ‘wet’ AMD. Wet AMD occurs when abnormal blood vessels grow underneath the retina.These unhealthy vessels leak blood and fluid, which can prevent the retina from working properly. Severe damage leads to severe permanent loss of central vision, but the eye is not usually at risk of losing all vision (going ‘blind’) as the ability to see in the periphery (side) remains. There is a less common form of late AMD called geographic atrophy, where vision is lost through the macular tissue becoming completely worn out, with no leaking blood vessels. Unfortunately, anti-angiogenic medicines cannot help this form of lateAMD.
What is myopic choroidal neovascularization?
This condition occurs in people who are highly myopic (short-sighted). When someone is highly short-sighted, the retina at the back of the eye is stretched due to the increased size of the eye. This stretching can make the retina thinner and prone to splitting. When this occurs, blood vessels from the choroid (the layer of the eye behind the retina) can grow underneath the retina. These new vessels (neovascularisation) leak blood and fluid, which can prevent the retina from working properly. Severe damage leads to severe permanent loss of centralvision.
What is diabetic macular oedema (DMO)?
Diabetic macular oedema is an eye condition occurring in people with both type 1 and type 2 diabetes. Macular oedema is swelling and thickening of the macula. The macula is a small area in the centre of the retina which contains a rich collection of nerve cells sensitive to light, fine detail, and colour DMO occurs as a result of changes in retinal blood vessels in people with diabetes. Diabetes is characterised by increased levels of sugar (glucose) in the blood stream. Consistently high blood sugar can damage blood vessels, with the first signs appearing in the smallest vessels, called capillaries. The damaged blood vessels will leak, causing the build-up of excess fluid (oedema) and blood in the macula. It can lead to severe impairment of central vision in the affected eye.
What is retinal vein occlusion (RVO)?
RVO occurs when one of the retinal veins is blocked. The retina is thelight sensitive tissue that lines the back of the eye and is responsible for eyesight. RVO usually occurs when:A retinal vein is ‘pinched off’ through the pressure of an artery lying on top of the vein; or is clogged with a blood clot or atherosclerotic plaque (fatty deposit in the wall of the artery); or is blocked by some inflammatory conditions. The block can occur in the main retinal vein-central retinal vein occlusion (CRVO), or in one of the branches of the main vein-branch retinal vein occlusion (BRVO). Macular oedema is swelling and thickening of the macula. The macula is a small area in the centre of the retina that contains a rich collection of nerve cells sensitive to light, fine detail, and colour. The vein block causes the blood pressure to increase in the small retinal blood vessels which causes them to bleed and leak fluid into the retina, forming a macular oedema. The retina may also be affected by poor blood flow and inflammation. All these processes lead to decrease/loss of vision in the affected eye.
Can I have treatment with anti-angiogenic (anti-VEGF) drugs if I am pregnant or breast-feeding?
If you are pregnant or planning to become pregnant, please discuss this with your doctor before your intravitreal injection treatment. Anti-VEGF medicines should be used with caution during pregnancy. Women of child-bearing potential should use effective contraception during their treatment and for at least three months after the last intravitreal injection. If you do become pregnant whilst undergoing intravitreal injections, please inform your doctor immediately. Anti-VEGF medicines are not recommended during breast-feeding because it is not known whether the medicine passes into human milk. Ask your doctor for advice before treatment.
Who else should not be treated with anti-VEGF?
You should not be given anti-VEGF treatment if you have any of the following:
- Allergy to anti-VEGF or any of its ingredients.
- An infection in or around either eye or severeinfectionanywhere in your body.Anti-VEGF should be used with caution in patients who have had a heart attack or stroke in the last three months, or who have uncontrolled angina or uncontrolled high blood pressure. Please ensure you inform the doctor if there are any changes in your medical condition.
How does an anti-VEGF injection prevent sight loss?
Anti-VEGF medicines stop the abnormal blood vessels growing, then leaking and bleeding under the retina. This prevents or limits damage to the retinal light receptors and loss of central vision. These medicines are effective in preventing further central vision loss in up to 90% of treated eyes.
Is anti-VEGF treatment right for me?
Your ophthalmologist will advise if the treatment is appropriate for you and which anti-VEGF medicine will be used. Only patients with active leaking of blood and fluid can benefit from it. The treatment that’s right for you will depend on the specific condition of your central retina (macula), your vision and whether there is scarring at the macula. We perform scans and photographs of the eye which show us the different layers of the retina. These scans can show us if there is blood or fluid present within the retinal layers and help us decide on your treatment.
How is the treatment given?
The drug is injected into your eye with a fine needle. Minimal discomfort is to be expected (equivalent to having blood taken from your arm). The procedure takes five to seven minutes, but the injection itself is over in less than 20 seconds. The injection is given with you lying down comfortably on the couch.Firstly, local anaesthetic drops are applied to numb your eye and minimise discomfort. Then, your eyelids and surface of the eye are cleaned to prevent infection. Your face and the area around your eye will be covered by a small surgical sheet (a drape) to keep the area sterile. A small clip (speculum) will be used to keep the eye open (see picture below). The injection site is marked with callipers and your eye is stabilised with forceps or a cotton bud. A few seconds later, the injection is given. The injecting clinician will use lubricating drops after your injection. Your vision is assessed post injection by checking you can see hand movementsor can countfingers.The image on the next page shows an eye draped with a speculum in place. The cotton bud is stabilising the eye while the injection is being given.
Who will give the injection?
These injections will be given either by an ophthalmologist or a registered nurse practitioner.
What are the side effects of injections?
As with any medical procedure, there is a small risk of complications following anti-VEGF treatment.
Some common side effects that could occur include:
- Red eye (there is usually a bleed or bruise on the white part of the eye at the site of injection, which clears in a week ortwo).
- Sore and gritty eye (slight ache and discomfort lasting a day or two).
- ‘Blobs’ or ‘small specks’ in your vision (‘floaters’) might be seen for a few days after the injection. You may also experience transient flashing lights or swirls of light immediately after the injection. It is important to note that most of the discomfort relating to injections is due to the use of Povidone Iodine antiseptic. This is a vital part of the injection process and reduces the risk of infection. Rare risks of anti-VEGF injections:
- serious eye infection (one in 2,000 cases).
- detached retina.
- increased eyepressure.
- blood clots and bleeding in theeye.
- inflammation inside theeye.There are no special precautions following intravitreal injections and you will be able to travel, but please avoid getting water into your eye or swimming for the first few days afterwards.
Types of Cataract Surgery
ECCE,SICS,PHACO,MICS
ECCE – Incision Size 10 to 12mm
- Requires Large Wound Space
- Requires Stitches
- Visual recovery takes longer time
- Requires long term post operative follow-up

In SICS – small Incision Cataract Surgery, 6mm Incision is made in the eye for cataract removal
- 6mm Incision size is required mostly
- Suitable for Rigid lens implant
- Require Stitches Rarely
- Visual recovery takes longer time
- Requires long – term post operative follow-up

In Phacoemulsification Ultrasound technology is used to break and Emulsify the Cataract through a 2.8mm Incision for the procedure. This smaller incision heals faster
- Smaller Incision is sufficient (2.8mm)
- Suitable for Foldable lens implant
- No stitches
- Instant visual recover
- Short term post operative follow-up

Micro Incision Cataract Surgery
This latest surgical technique involves only 1.4mm incision in the eye for cataract removal with the ultrasound phaco technology.
- Very tiny wound is made (1.4mm)
- IOL can be implanted through 1.8mm
- No stitches
- Walk in – Walk out, visual recovery is fastest
- Short term post operative follow-up
- Advanced technique
- Minimally invasive
- Better functional vision

| Normal Vision | Vision with Cataract |
|---|---|
 |
 |
When is the best time to treat cataracts?
What happens if cataracts go untreated?
Can cataracts come back?
How successful is a cataract surger?
How do i know which lens implant is right for me?
What is presbyopia?
What is a multifocal lens?
When is the best time to treat cataracts?
Many people believe cataracts have to be ‘ripe’ before they can be removed. This is no longer true. Today, cataract surgery is a routine procedure that can be performed as soon as your vision interferes with the quality of your life.
What happens if cataracts go untreated?
Over time , the clouded areas of your lens can become larger and more dense, causing your sight to become worse. This could take anywhere from a few months to many years. Eventually, your entire lens can cloud over leading to blindness.
Can cataracts come back?
Once a cataract has been removed it cannot return. However , over time some patients may complain that their vision has once again become cloudy. This condition is known as secondary cataract. It can be easily and rapidly treated by a simple laser procedure performed in the office.
How successful is a cataract surger?
Cataract surgery has a overall success rate of 99% or greater. Continuous innovations in techniques and instruments have made the procedure safer than earlier.
How do i know which lens implant is right for me?
No single lens works best for everyone and only your ophthalmologist can determine the most appropriate option for you.
When is the best time to treat cataracts?
Many people believe cataracts have to be ‘ripe’ before they can be removed. This is no longer true. Today, cataract surgery is a routine procedure that can be performed as soon as your vision interferes with the quality of your life.
What is presbyopia?
Presbyopia is the condition in which the lens of the eye loses its ability to focus. It is a common condition that could accompany cataracts and impair your ability to see objects that are close up.
Have you ever found yourself holding a menu or book farther away to read it? the need for reading glasses is usually a sign of presbyopia. This aging of the eyes eventually affects everyone. If you have cataracts with presbyopia, the lens can correct both conditions.
What is a multifocal lens?
Multifocal lens is a breakthrough lens for cataract surgery that lets patient see from near to far, usually without glasses. It is effective when placed in both eyes. Most of the multifocal lens patients find that they can read a book, work on the computer, drive a car – day or night – and play golf or tennis with an increased freedom from glasses. You my experience visual disturbances in low lighting conditions, therefore increased care should be taken when driving at night
Cataract Natural Part
A NATURAL PART OF AGING
The natural lens, located behind the iris, works just like the lens of a camera focusing light images on the retina which sends images to the brain.With the onset of cataract, your natural lens becomes so clouded that it prevents light and images from reaching the retina. You now start seeing objects blurred. Bright colours seem dull. Seeing during low light conditions become more difficult, your glasses become in effective.
| Healthy EYE | EYE with Cataract |
|
|
What causes Cataract?
- Normal aging process
- Diabetics may cause
- Injury
- Prologed use of medication (eg : steroids)
- The best way to treat cataract is with surgery which removes the old, clouded lens and replaces it with a new, artificial one to restore your vision. Successful cataract surgery can significantly improve your quality of life.
What exactly is cataract surgery?
- It is one of the safest and most successful procedure
- Surgery is performed mostly under local anaesthesia rarely needs general anaesthesis
- Modern surgery uses an ultrasound (phacoemulsification) to remove the cataract
- Artificial lens is placed in to the eye
- The surgery is performed without stitches
- It takes 15-45 minutes
- Safe and effective
- The risk of complication is less than 1%
Lens Options
| Near Vision | Intemediate Vision | Distance | |
Monofocal LensA lens with a single focal point, designed to replace |
 |
 |
 |
AsphericLens For enhanced contrast & Better Night vision |
 |
 |
 |
Cataract + AstigmatismAstigmatism correcting Monofocal Lens A lens with a single focal point, designated to replace Cataracteous lens and pre – existing astigmatism, providing distance vision, while offering enhanced image quality. |
 |
 |
 |
Multifocal IOL |
 |
 |
 |
Retinal Detachment (RD)
WHAT IS RETINAL DETACHMENT?
When the retina is pulled on lifted from its normal position it results in a detachment. This causes permanent vision loss if not treated immediately. This is a medical emergency and should be treated immediately.
What are the symptoms of retinal detachment?
- Sudden or gradual increase in floaters
- Flashes of light
- Appearance of a curtain over the field of vision
Who is at risk of retinal detachment?
- It can occur at any age but people over 40 are at a higher risk.
- Men are more prone to it than women.
- People who are extremely near sighted.
- People with a family history of retinal detachment.
- People with other eye diseases or injuries.
Computer Vision Syndrome (CVS)
WHAT IS COMPUTER VISION SYNDROME?
A number of professionals using computers experience vision and eye related problems especially due to poorly designed work stations and prolonged usage. These vision related problems are grouped as Computer Vision syndrome in short “CVS”.
- What are its symptoms?
- Who is affected? How?
- What are the reasons?
- What does computer vision clinic do?
What are its symptoms?
- Eye strain
- Blurred vision
- Dry and irritated tired eyes
- Headaches
- Neck and backaches
Who is affected? How?
Computer Vision Syndrome ( CVS ) affects 75% of the computer users, most markedly those who work more than 3 to 4 hours with computers. Computer users? productivity is affected.
What are the reasons?
- Uncorrected refractive error
- Decreased blink rate
- Glare and reflection from the monitor
- Poor Ergonomics
What does computer vision clinic do?
Evaluate at simulated computer environment ( Questionnaire + Executive Vision check + Orthoptics + Tear
- Management
- Glass
- Artificial tears
- Vision therapy
- Recommendations about ergonomics
WHAT IS CORNEAL GRAFTING?
When cornea is damaged beyond repair it is removed either fully or partly and replaced by a donated cornea.
- What is the cornea?
- Who will require corneal graft?
- Who can donate corneas?
- What should we do after the surgery?
What is the cornea?
Cornea is the clear outer layer covering the eye. It helps focus and transmit light as it passes through the lens on to retina.
Who will require corneal graft?
People with congenital abnormalities that inhibits normal vision.People with clouded corneas through childhood diseases, trauma or infections.People with degenerative eye diseases that cause loss of vision.
Who can donate corneas?
Anyone with no infectious diseases.
What should we do after the surgery?
Do not rub or touch the eye.Avoid smoky and dusty rooms, which can cause irritation.
Wear sunglasses if the eye is light sensitive.Do not play contact sports and swimming in particular. Ask the doctor if you are unclear which sports you should avoid.You will need at least 2-4 weeks off work, but again this will be discussed with you on an individual basis.Avoid driving until the doctor tells you otherwise.Consult your doctor in case of increased pain, redness, watering or discharge or reduction of vision
DOES DIABETES CAUSE EYE PROBLEMS?
Yes. Some of the diseases it causes are diabetic retinopathy, glaucoma, cataract, infections, and refractive errors.
What are the symptoms of diabetic retinopathy?
No symptoms at the early stage. Increase in floaters and even mild reduction in vision should be evaluated in diabetic patients.
Implantable Contact Lens (ICL)
How do I know if I am a suitable ICL candidate?
Candidates for the ICL are between 21 and 45 years of age, suffer from myopia (nearsightedness),
hyperopia (farsightedness) and/or astigmatism (cylindrical power) and want to experience superior vision correction. The ideal ICL candidate has not undergone any ophthalmic surgery (though your surgeon might opt to do it as a secondary procedure in certain select cases) and does not have a history of eye disease such as iritis, glaucoma, or diabetic retinopathy.
Nearly anyone seeking clearer vision may be a ICL candidate, including those with special or extreme vision correction needs. Prospective person should consult his/her ophthalmologist (eye surgeon) for more information, including an assessment of their candidacy.
Women who are pregnant or nursing should wait to have the ICL implanted. Lastly, those without a large enough anterior chamber depth or endothelial cell density may not be a good ICL candidate.
Where is the ICL placed?
A trained ophthalmologist will insert the ICL through a small micro-incison, placing it inside the eye just behind the iris in front of the eye’s natural lens. The ICL is designed not to touch any internal eye structures and stay in place with no special care.
What is Toric ICL?
The Toric ICL is a only variant of ICL. Toric ICL corrects your nearsightedness as well as your
astigmatism (cylindrical power) in one single procedure. Each lens is custom made to meet the needs of each individual eye.
Does it hurt?
No, most patients state that they are very comfortable throughout the procedure. Your ophthalmologist will use a topical anesthetic drop prior to the procedure and may choose to administer a light sedative as well.
What is the ICL made of?
The ICL is made of Collamer®, a highly biocompatible advanced lens material which contains a small amount of purified collagen. Collamer does not cause a reaction inside the eye and it contains an ultraviolet filter that provides protection to the eye. Collamer is a material proprietary to STAAR Surgical Company, the company that manufactures ICL.
What if my vision changes after I receive the ICL?
One advantage of the ICL is that it offers treatment flexibility. If your vision changes dramatically after receiving the implant, your doctor can remove and replace it. If necessary, another procedure can be performed at any time.
Patients can wear glasses or contact lenses as needed following treatment with the ICL. The implant does not treat presbyopia (difficulty with reading in people 40 and older), but you can use reading glasses as needed after receiving the ICL.
What type of procedure is involved in implanting the ICL?
The implantation procedure for the ICL (Implantable Contact Lens) is refractive eye surgery that involves a procedure similar to the intraocular lens (IOL) implantation performed during cataract surgery. The main difference is that, unlike cataract surgery, the ICL eye surgery does not require the removal of the eye’s natural lens. The ICL procedure is a relatively short outpatient procedure that involves several important steps. The surgical procedure to implant the ICL is simple and nearly painless.
As a ICL candidate, your doctor will prepare your eyes one to two weeks prior to surgery by using a laser to create a small opening between the lens and the front chamber of your eye (iridotomy). This allows fluid to pass between the two areas, thereby avoiding the buildup of intraocular pressure following the surgery.
However, some surgeons choose to do this step on the same day of the surgery.The implantation procedure itself takes about 15-30 minutes and is performed on an outpatient basis, though you will have to make arrangements for someone to drive you to and from the procedure. You can expect to experience very little discomfort during the ICL implantation. You will undergo treatment while under a light topical or local anesthetic, perhaps with the addition of a mild sedative.
Following surgery, you may use prescription eye drops or oral medication. The day after surgery, you will return to your doctor for a follow-up visit. You will also have follow-up visits one month and six months following the procedure. Although the ICL requires no special maintenance, you are encouraged to visit your eye doctor annually for check-ups following the ICL procedure.
Can the ICL be removed from my eye?
Although the ICL is intended to remain in place permanently, a certified ophthalmologist can remove the implant in a very quick & short procedure.
Is the ICL visible to others?
No, the ICL is positioned behind the iris (the colored part of the eye), where it is invisible to both you and observers. Only your doctor will be able to tell that vision correction has taken place.
Will I be able to feel the ICL once it is in place?
The ICL is designed to be completely unobtrusive after it is put in place. It stays in position by itself and does not interact with any of the eye’s structures.
Where can I get my ICL procedure done?
Please be aware that ICL procedure is presently available at select centres & hospitals in India as it requires precision and skills. In our Hospital, Dr Anand Shroff, our Cornea and LASIK expert will guide you better if you are the right candidate for this procedure.
What is the surety that I would not get back any of the numbers after the treatment? That is, is this a permanent solution? I would not be required to wear any lenses / specs after the treatment?
The same surety that you could hand me today that your spectacle powers will not change!. Please remember that the eye is an organ not doing static fixed focus work, but something dynamic. If powers shift in adulthood, these are usually not related to the shape of your eyes or measurements taken of the same. These are also largely due to lifestyle, working long hours on the PC, changing the utility of your visual work from computers to movie screens etc.
Our duty is to make you aware that doing such activities without proper and necessary precautions will shift your powers slightly (not hugely, but yes, small powers may come into play).
This is the reason why we shall insist that you use computer specific prescription when working long hours on the PC, take frequent breaks etc.
Would there be any reaction due to the lenses being implanted – like my eyes not accepting the lenses, irritation in eyes, itchiness etc.
In our experience, we have not seen any adverse effects. Itchiness of the eyes is usually in the eye lids, this part is untouched in ICL or LASIK treatments. hence, if your eyes are prone to turning ‘red’ or getting ‘itchy’ or ‘dry’ this is the inherent nature of your eyes and the procedure does not aggravate or cause this.
Since I am working, I need to plan my days off from work. So, how many days rest am I required to take post treatment?
If planned well, no more than 10 days are required for doing ICL as both eyes are not treated on the same day.
All options will be discussed during the LASIK evaluation to determine which technology is most appropriate for you.
Macular Degeneration
What is Macular Degeneration?
Age-related Macular degeneration (AMD) is a disease associated with aging that gradually destroys sharp, central vision. The disease attacks the macula, the central area of the retina that allows a person to see fine detail. Individuals can lose all but the outermost peripheral vision, leaving dim images or black holes at the center of vision. Central vision is needed is needed for seeing objects clearly and for common daily tasks such as reading, driving, identifying faces and watching television. AMD is a leading cause of vision loss and legal blindness in adults over 60 in the United States.

Two Types of Macular Degeneration
Macular degeneration is diagnosed as either dry or wet. Dry AMD is more common than wet AMD, with about 90% of people having the dry type and 10% of people having the wet type. However, even though the wet type is less common, 90% of severe vision loss comes from the wet type and only 10% from the dry type.
Dry AMD
Dry AMD occurs when the light-sensitive cells in the macula slowly break down, gradually blurring central vision in the affected eye. It is diagnosed when yellow deposits known as drusen accumulate in the macula. Dry AMD causes gradual central vision loss, but the loss usually is not as severe as can be found with the wet type.
Wet AMD
Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula. These new blood vessels tend to be very fragile and often leak blood and fluid. This blood and fluid raises the macula from its normal place at the back of the eye, causing scarring and permanent damage to light-sensitive retinal cells, which creates blind or blurry spots in the central vision.
Cause of AMD
The cause of AMD is not complemtely known. However, the greatest risk factor is age. The risk of having AMD increases with age, from 10% at age 50 to about 30% at age 75. Other factors that increase the risk of developing AMD include family history of AMD, smoking, diet, weight and race. Caucasians are much more likely to lose vision from AMD than other races (*NIH). Lifestyle practices like not smoking, eating a healthy diet high in green leafy vegetables and fish, exercising and maintaining normal weight and blood pressure may play a role in reducing the risk of developing AMD.
Symptoms
Especially with the dry form, symptoms may develop gradually. Also if only one eye is affected, a person may not notice changes in vision until the disease gets moderately worse because the unaffected eye helps to compensate for changes in vision. Having an annual eye exam is very important for detecting AMD and other ocular disorders early in their progression
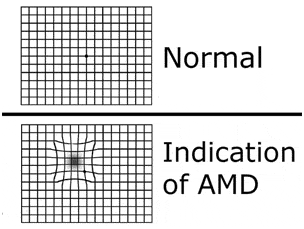
Symptoms of AMD may include blurred vision, a dark area or “blind spot”, or a distorted appearance of straight lines or other objects. It is important for people with AMD to monitor their vision closely and to call their eye doctor if there is a change in vision. One way to monitor vision or detect a problem is with an Amsler grid. The Amsler grid, which looks similar to a section of graph paper, is a diagnostic tool that aids in the detection of visual disturbances caused by changes in the retina. The Amsler grid is a very sensitive test that can reveal clinical changes before other visual symptoms develop. With new and reliable treatments for wet AMD, this tool is important for the early detection of wet AMD..
Treatment
Dry AMD
The National Eye Institute’s Age-Related Eye Disease Study (AREDS) found that taking a specific high-dose formulation of antioxidants and zinc can reduce the risk of progression of dry AMD in some patients. The AREDS formulation is not a cure for AMD. It will not restore vision already lost from the disease. However, it may delay the onset of advanced AMD. It may also help people who are at high risk for developing advanced AMD keep their vision.
Wet AMD
Wet AMD can be treated with laser therapy, photodynamic therapy, and injections into the eye. Some patients receive one of these treatments and some patients receive a combination of these treatments. None of these treatments is a cure for wet AMD, but they may halt the progression of the disease and in some cases allow for some gain in visual acuity.
Laser Therapy
This procedure uses a high energy beam of light to seal or destroy the abnormal blood vessels to prevent leaking and further loss of vision. However, laser treatment may also destroy some surrounding healthy tissue and some vision. Therefore, only a small percentage of people with wet AMD are treated with laser surgery- mainly those whose leaky blood vessels have developed away from the central part of the macula. The risk of new blood vessels developing after laser treatment is high and repeated treatments may be necessary.
Photodynamic Therapy
This procedure uses a combination of light and drug therapy to destroy leaking blood vessels. First a drug called Verteporfin is injected into a patients arm. It travels throughout the body, including to the eye, where it “sticks” to the surface of new leaky blood vessels. Next, a light is shone into the eye for about 90 seconds. The light activates the drug which destroys the new blood vessels, leading to a slower rate of visual decline. Unlike laser surgery, the drug does not destroy surrounding healthy tissue. This therapy slows the rate of vision loss, but does not stop vision loss altogether or restore vision in eyes already damaged by AMD. Treatment results are often temporary and may need to be repeated.
Anti-VEGF Therapy (Intravitreal Injections)
The treatment of AMD has evolved in the last 5 or so years from limiting the degree of vision loss to maintaining and even improving existing vision in some cases. This is due in no small part to Anti-VEGF (Vascular Endothelial Growth Factor) therapy. Anti-VEGF therapy works by blocking the action of VEGF, the molecule that promotes the growth of abnormal blood vessels under the retina. These drugs are injected directly inside the eye to provide maximum concentration in the area where they are needed. The eye is numbed before each injection. There may be slight discomfort and soreness on the day of the injection, but not pain. Multiple injections will be given as often as monthly, with the goal of achieving up to 3 to 6 months between injections. These drugs maintain vision in up to 90% of all patients treated. Vision may improve in up to 1/3 of treated patients.
Diabetic Eye Disease
What Is Diabetic Eye Disease (Diabetic Retinopathy)?
With diabetes, the body can’t use or store sugar properly. Diabetes damages the blood vessels in the eye. The damage of the blood vessels causes diabetic retinopathy. In later stages, the disease may lead to new blood vessel growth over the retina. The new blood vessels can cause scar tissue to develop, which can pull the retina away from the back of the eye. This is known as retinal detachment, and it can lead to blindness if untreated. The presence and severity of diabetic retinopathy is related to the duration of diabetes. However, severe and significant diabetic retinopathy can be present at the time of diagnosis especially with adult onset diabetes.
Signs And Symptoms Of Diabetic Retinopathy
Everyone who has diabetes is at risk for developing diabetic retinopathy. In the early or advanced stages of diabetes, symptoms may be absent or minimal. Therefore, regular diabetic screening evaluations are recommended. The symptoms of diabetic retinopathy can include floaters, blurred vision or double vision. Sometimes difficulty reading or doing close work can indicate that fluid is collecting in the macula, the most light-sensitive part of the retina. This fluid buildup is called macular edema.
Treatment Of Diabetic Retinopathy
The severity of diabetic retinopathy can be limited or prevented by close monitoring and control of blood sugars, blood pressures and blood lipids, such as cholesterol. Control of any one of these risk factors can reduce the severity of diabetic retinopathy. According to the American Academy of Ophthalmology, 95% of those with significant diabetic retinopathy can avoid substantial vision loss if they are treated in time. The possibility of early detection is why it is so important for diabetics to have a dilated eye exam at least once a year. Diabetic retinopathy can be treated with laser photocoagulation to seal off leaking blood vessels and destroy new growth. Laser photocoagulation doesn’t cause pain, because the retina does not contain nerve endings. In some patients, blood leaks into the vitreous humor and clouds vision. A procedure called a vitrectomy removes blood that has leaked into the vitreous humor. The body gradually replaces lost vitreous humor, and vision usually improves.
Glaucoma
Glaucoma is a condition that results in slow progressive damage to the optic nerve, which sends information from the eye to the brain. Damage to the optic nerve leads to a slow loss of vision. As a result, glaucoma is often referred to as The Silent Thief of Sight. Rick factors for glaucoma include elevated eye pressure, increased age, African-American heritage, and previous ocular injury. The most important and most treatable risk factor for glaucoma is elevated eye pressure. Inside the eye, there is a constant production of fluid that normally flows out of the eye through a very small drain. In certain individuals, this drain can become blocked for various reasons. The result is an increase in eye pressure, therefore increasing your risk of glaucoma. Glaucoma affects an estimated 3 million Americans and is the second-leading cause of blindness in the United States.
Types of Glaucoma
Open-Angle Glaucoma
Open-Angle Glaucoma: Open-angle glaucoma occurs slowly as the drainage area in the eye becomes clogged. Pressure builds up when the fluid inside the eye is unable to drain. Side (peripheral) vision is damaged gradually. Open-angle glaucoma is the most common kind of glaucoma.
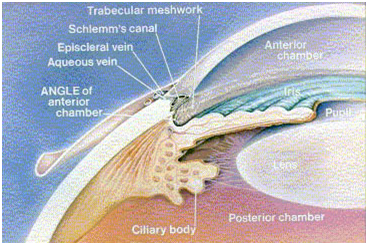
Closed-Angle Glaucoma
Closed-Angle Glaucoma: With closed-angle glaucoma, eye pressure builds up rapidly when the drainage area of the eye suddenly becomes blocked. Blurry vision, rainbow halos around lights, headaches or severe pain may occur with closed-angle glaucoma. This type of glaucoma is less common than open-angle and may cause blindness if it is not treated immediately.

Questions and Answers
What is the best way to detect glaucoma?
Careful examination of the optic nerve coupled with visual field testing and intraocular pressure measurement provides the necessary information to determine if damage from glaucoma is present.
If I am having no visual or ocular problems, can I be certain that I do not have glaucoma?
No. In fact, people with significant levels of damage may not have visual symptoms until most of the optic nerve function is lost. This is because the disease process is generally very slow, giving glaucoma the nickname “The Silent Thief of Sight”. In most cases, damage occurs to side (peripheral) vision first, and one eye may have significant field loss, but the other does not, so with both eyes open a person may not realize the extent of the damage.
What can I do to reduce my risk of further damage?
The two most important things you can do if you are diagnosed with glaucoma are to keep follow-up appointments and faithfully use ocular medications as prescribed. Careful monitoring and consistent treatment can often stabilize this disease process.
LASIK
Refractive Disorders
In a normal eye, light entering the eye is refracted (bent) first by the eye’s cornea and then by the eye’s natural lens so that it focuses precisely on the retina. The retina is the sensitive tissue on the back of the eye that converts light images into electrical impulses and sends them through the optic nerve to the brain. If the light rays are not focused precisely on the retina, the result is refractive error, or poor vision in the form of nearsightedness, farsightedness or astigmatism.
Nearsightedness (myopia)
Nearsightedness occurs when the eye’s cornea is shaped too steeply, or the eye is too long. Incoming light rays are refracted to a focal point in front of the retina instead of on the retina. This results in distant objects being out of focus, while close objects can be seen clearly.
Farsightedness (hyperopia)
Farsightedness is the reverse of nearsightedness. Instead of a cornea that is too steep, the farsighted eye has a cornea that is too flat, or the eye is too short. Light rays refracted through the cornea converge at a focal point behind the retina. This results in close objects being out of focus while distant objects are more clear.
Astigmatism
Astigmatism is the result of an aspheric (irregularly shaped) cornea that scatters light rays as they enter the eye. An astigmatic cornea has an oblong shape like a football instead of a round shape like a basketball. The result is that there is no single focal point, and vision is blurry both near and far.
Presbyopia
Presbyopia refers to the normal process of aging in which the natural lens inside the eye becomes hardened. As this occurs, the lens loses its flexibility, which makes reading difficult. This usually occurs between the ages of 40 and 50. Everyone experiences presbyopia. The result of this normal process is bifocals for those who wear glasses or contacts, and reading glasses for those who have not needed corrective lenses previously. LASIK surgery will not correct presbyopia.
Correcting Refractive Disorders
Wearing corrective lenses merely treats the symptoms of nearsightedness, farsightedness and astigmatism. The lenses do not correct the refractive error. Those with nearsightedness, farsightedness and astigmatism can benefit from refractive surgery because refractive surgery corrects the error by enhancing the eye’s ability to refract light rays precisely onto the retina.
Many people think that LASIK is the only type of refractive surgery, and today LASIK is the most commonly performed corrective eye surgery in the United States, but in truth, there are many different procedures to choose from. Refractive surgery, also known as corrective eye surgery, encompasses a multitude of procedures designed to treat and correct refractive errors including nearsightedness, farsightedness and astigmatism. In each of these procedures, a laser is used to reshape the cornea to alter the way light rays enter the eye to achieve focus. The process used, however, differs from surgeon to surgeon.
LASIK
Laser in situ keratomileusis, or LASIK, is the most commonly performed refractive surgery procedure today and is the primary procedure of choice at Wolfe Eye Clinic. LASIK has advantages over other procedures, including a relative lack of pain and the fact that good vision is usually achieved almost immediately or in a very short period of time. Those with nearsightedness, farsightedness and astigmatism can benefit from LASIK. During LASIK surgery, a thin flap of tissue is created on the center of the cornea (Figure 1). This flap is then lifted back to expose the internal tissue, or stroma, of the cornea. An excimer laser is then used to reshape the cornea and correct the refractive disorder (Figure 2). The flap is then layed back over the cornea where it heals itself in a very short period of time (Figure 3).
With LASIK, the instrument used to create the flap varies. Most surgeons use an instrument called a microkeratome. A microkeratome is a device that uses a very sharp oscillating blade to cut the flap. Other surgeons, including those at Wolfe Eye Clinic, prefer a more advanced bladeless technique, using a very precise laser to create the flap instead. Wolfe Eye Clinic surgeons use the IntraLase laser to create the flap during LASIK surgery.
The Zyoptix z-100 is a major advance in treatment. It has advanced safety features that include iris recognition that ensures treatment for the correct eye and rotational eye tracker that ensures greater precision. This treatment is twice as fast and is suitable for a greater variety of abnormalities. It affords excellent results.
The advantages include:
- Iris Recognition- Greater accuracy of treatment placement
- Automatic patient identification ensures correct eye is treated
- Zy-ID – A unique digital ‘map’ of the iris, individual to every patient
- Multidimensional Eye tracker- Compensates and corrects for intra-operative eye-movement in every dimension, including cyclotorsion and pupil shift
- 100Hz Laser- For significantly faster treatment times
- Treatment planner- For wide range of treatment options
- LED Illuminations- For greater pupil iris contrast, greater surgical visibility and improved comfort for patients and surgeons
- Zeiss Microscope- Increases visibility by allowing for 3 levels of magnification.
- With the latest technology at the hands of skilled professionals, the Centre ensures the best results possible.
PRK
Photorefractive keratectomy, or PRK, was the first refractive procedure that utilized the excimer laser to reshape the front surface of the cornea. It was initially envisioned in 1983 and, after a long series of clinical trials, was approved by the FDA in 1995. PRK however is primarily used to correct mild to moderate cases of nearsightedness and astigmatism. After the eye has been anesthetized with topical eye drops, your doctor prepares the eye by removing the surface layer of the cornea called the epithelium. This layer naturally regenerates itself every few days. Pulses of laser light are then applied to the surface of the cornea to reshape the curvature of the eye. Postoperatively, patients typically wear a bandage contact lens for the first three to five days to reduce postoperative pain and irritation. Anti-inflammatory eye drops are used in a decreasing dose for several months. Vision is usually blurry initially and starts to clear over the first several weeks, while continuing to improve for up to one year.
LASEK
Laser Epithelial keratomileusis, or LASEK, is a laser procedure that is used mostly for people with corneas that are too thin or too flat for traditional LASIK. It was developed to reduce the chance of complications that occur when the flap created during LASIK is not the ideal thickness or diameter. In LASEK, the epithelium, or outer layer of the cornea, is cut not with the microkeratome blade or laser used in LASIK, but with a blade called a trephine. Next, the surgeon covers the eye with an alcohol solution for around 30 seconds. The solution loosens the edges of the epithelium. After sponging the alcohol solution from the eye, the surgeon uses a tiny tool to lift the edge of the epithelial flap and fold it back out of the way. Then the surgeon uses an excimer laser, as in LASIK or PRK, to apply pulses of laser light that sculpt the corneal tissue underneath. Afterward, the epithelial flap is placed back on the eye. There is a possibility of a reaction to the alcohol that may kill some of the epithelial cells. Patients typically wear a bandage contact lens for around four days and may feel eye irritation during the first few days afterward. The time it takes to recover good vision is up to four to seven days longer than with LASIK.
Epi-LASIK
Epi-LASIK is a cross between LASIK and LASEK. During Epi-LASIK, a flap is cut in the cornea’s outer layer, just as in LASIK and LASEK. However, with Epi-LASIK the surgeon uses a blunt, plastic oscillating blade. Instead of the alcohol that is used in LASEK to loosen the epithelial sheet, during Epi-LASIK the surgeon uses the blunt plastic blade, called an epithelial separator, to scrape the sheet across the eye. Next, the surgeon uses an excimer laser, as in LASIK, LASEK or PRK, to apply pulses of laser light that sculpt the corneal tissue underneath. Afterward, the epithelial flap is placed back on the eye. Then, a special contact lens is placed on the eye to keep the flap in place while it re-epithelializes. Vision will probably be cloudy or variable at first, unlike traditional LASIK. Some patients report good vision within a week or two, while others take three to six months to reach their final result. These recovery times are significantly longer than with LASIK, which usually allows people to achieve good vision from the same day up to a few weeks later and to drive by the day afterward.
Lens Implants — An Alternative to LASIK

LASIK surgery is not an option for everyone. A very high refractive error, thin corneas or severe dry eye may prohibit someone from being a good LASIK candidate. Fortunately, implantable lenses may provide an alternative. Examples of these lenses include the Verisyse™ Intraocular Lens, Visian’s Intraocular Collamer Lens, Alcon’s Acrysof® ReSTOR® Intraocular Lens and the ReZoom™ multi-focal Intraocular Lens. Unlike LASIK, which reshapes the outer part of the eye, lens implants are inserted inside the eye. Once in place, the lens stays in place indefinitely and should require no maintenance.


