Paediatric Surgery FAQ’s
What is the focus of pediatric surgery?
Pediatric surgeons utilize their expertise in providing surgical care for all problems or conditions affecting children that require surgical intervention. They participate in transplantation operations, and like most surgeons today, they use laparoscopic techniques for some operations.
They also have particular expertise in the following areas of responsibility:
- Neonatal– Pediatric surgeons have specialized knowledge in the surgical repair of birth defects, some of which may be life threatening to premature and full-term infants.
- Prenatal– Pediatric surgeons, in cooperation with radiologists, use ultrasound and other technologies during the fetal stage of a child’s development to detect any abnormalities. They can then plan corrective surgery and educate and get to know parents before their baby is born. Prenatal diagnosis may lead to fetal surgery, which is a new forefront in the subspecialty of pediatric surgery. Application of most fetal surgical techniques is still in the experimental stage.
- Trauma– Because trauma is the number one killer of children in the World, pediatric surgeons are routinely faced with critical care situations involving traumatic injuries sustained by children that may or may not require surgical intervention. Many pediatric surgeons are involved in accident prevention programs in their communities that are aimed at curbing traumatic injuries in children.
- Pediatric Oncology– Pediatric surgeons are involved in the diagnosis and surgical care of children with malignant tumors as well as those with benign growths.
What is a Pediatric Surgeon?
Surgeons who specialize in general surgery often provide surgical care for children, and they are fully qualified to perform many operations on children.
Pediatric surgeons operate on children whose development ranges from the newborn stage through the teenage years. In addition to completing training and achieving board certification, pediatric surgeons complete two additional years of training exclusively in children’s surgery. They then receive special certification in the subspecialty of pediatric surgery.
What is the pediatric surgeon’s role in treating the child?
Pediatric surgeons are primarily concerned with the diagnosis, preoperative, operative, and postoperative management of surgical problems in children. Some medical conditions in newborns are not compatible with a good quality of life unless these problems are corrected surgically.
These conditions must be recognized immediately by neonatologists, pediatricians, and family physicians. Pediatric surgeons cooperate with all of the specialists involved in a child’s medical care to determine whether surgery is the best option for the child.
Who administers my child’s anesthesia?
Your child’s anesthetic is supervised at all times by an anesthesiologist who has received specialty training in Pediatric Anesthesia. They will meet you at your child’s pre-operative (“Pre-care”) evaluation or on the morning of their surgery.
Will my child need blood tests before surgery?
Most healthy infants or children will not require any major pre-operative tests or bloodwork.
What will you do if my Child is Anxious before Surgery?
Medications are available that will sedate your child prior to the start of the anesthetic. These medications are similar to Valium® but are shorter acting. These medications can be given either by mouth or through an IV. In some institutions, induction rooms are available for the child to be with their parents while going off to sleep. Your anesthesiologist will decide what the best is for your child after discussion with you. A vast majority of children do not require anything other than a wagon to ride in and a hand to hold.
Will my child gets an IV before surgery?
For most children having outpatient surgery, the IV will be started after the child is asleep by inhaled anesthesia.
When will my child be able to go home?
If you child is having minor surgery, s/he may be able to go home a few hours after the procedure. Your child’s healthcare team will make sure that s/he is fully awake, that vital signs (i.e. heart and breathing rates, temperature, and blood pressure) are normal, and the s/he can take some liquids by mouth without vomiting.
What should my child eat after surgery?
Children sometimes vomit after surgery. Encourage your child to drink liquids, and then offer small amounts of bland food. Your child may then progress to a regular diet.
What can I expect when I take my child home?
You may notice that your child is sleeping more than usual for the first day or two. Also, your child may have some nausea and vomiting, or lack of appetite. These problems are usually related to anesthesia and should improve within 24 to 48 hours at home.
Common Paediatric Surgical Problems
- Congenital Diaphragmatic Hernia (CDH)
- Oesophageal atresia/sTracheo oesophageal fistula (TOF)
- Small Bowel Atresia
- Hirschsprung’s Disease
- Anorectal malformation,
- Exomphalos
- Gastroschisis
- Congenital Cystic Adenomatoid Malformation (CCAM)
- Necrotising enterocolitis (NEC)
- Pyloric stenosis
- Intusussception
- Appendicitis
Inguinal hernia / hydrocele Undescended Testis
The testis is responsible for sperm production in men. The general body temperature is 36.9o C. But sperm production is best at a temperature 2o less than this level. This is the reason why the testes are located outside the body.
When the baby is formed in the womb, the testis is initially formed inside the baby’s belly. As the fetus (baby in the womb) grows, the testes gradually descend out of the body and reach the sac (scrotum). When this does not happen, or is arrested half way, the result is ‘Undescended Testis’ (UDT).
- How common is Undescended Testis? Is it possible for the testis to descend by itself?
- How is it detected?
- What happens when Undescended Testis is not corrected?
- What is the right time to operate and bring down the testis (Orchidopexy)
- What are the complications of Orchidopexy?
- What are the chances of fertility after operation?
- What is a retractile testis?
- Can a normally descended testis go back up?
How common is Undescended Testis? Is it possible for the testis to descend by itself?
Undescended Testis is seen in 30% of boys born before date (preterm). In such cases it is very likely that testis can descend by itself in 3-6 months time. Among full term boys 1-3% are found to have Undescended Testis. They also have a small chance to correct this problem by themselves. But this possibility becomes much less after 6 months of age, after this age surgery is required to correct it.
How is it detected?
When the newborn baby is examined by the paediatrician, by feeling with hands one can find out that the testis is missing. When the sac (scrotum) is poorly formed, one can suspect this. Also parents can detect it in a similar way when bathing the child. When the testis is not there, one can wait for 3-6 months for spontaneous descent. If this does not happen, it is essential to consult a Paediatric Urologist.
What happens when Undescended Testis is not corrected?
- Infertility: As mentioned before, sperm production takes place at a lower temperature than body temperature. When testis is not descended, it is exposed to higher body temperature, and sperm production is affected. In later life these patients have much reduced sperm count and chance to father (50-70% less than normal).
- Twisting of Testis (Torsion): When the testis is not descended, it is very free to move around itself. This makes it easy to twist and cut off its own blood supply; the result being loss of testis.
- Testicular Tumor: There is a small risk of tumor development in Undescended Testis. By doing an operation to bring it down this can be easily checked out. If the testis is not brought down, tumor can develop without being noticed and can become advanced before treatment.
What is the right time to operate and bring down the testis (Orchidopexy)?
For the children with Undescended Testis, it is recommended to have surgical correction within one year to prevent infertility in later life. During this operation, the testis is found at the lower part of the belly and fixed to the testis after achieving enough length. When the testis is developed poorly, it may need to be removed. Some times the testis is absent by birth. Laparoscopy is essential in such situations. Also when the testis is too high, two-stage operation may be needed. During the first stage the blood supply to the testis is cut off using a laparoscope. As the testis develops new blood supply, it is brought down at a second stage. All these need to be carefully decided by the Paediatric Urologist.
What are the complications of Orchidopexy?
In general in 95% of such operations there is a successful outcome. In 5% the following complications can occur.
- Testis being small (Atrophy): This can result because of damage to the blood supply during the operation. This can also be a result of testis being small by birth.
- Testis going back up (Ascent): When the length is not enough and the testis is under tension, testis can go back high again.
What are the chances of fertility after operation?
When only one testis is affected, and surgery is performed at the right time, there is 80% chance for fertility and paternity. When both testis are affected, if the surgery is performed at the right time, there is still 50% chance for fertility and paternity.
What is a retractile testis?
Sometimes the testis intermittently disappears upwards. This phenomenon is called ‘retractile testis’. In this situation one can wait for the boy to grow, however a careful followup is essential. On regular followup checks if the testis prefers to stay higher or if the testis is under tension when brought down, surgical correction is recommended.
Can a normally descended testis go back up?
In some boys who had normal testis at birth, at a later age the testis can go back up. This is called ‘ascending testis’. This is due to increased activity of a muscle around the cord. Although it can be an intermittent phenomenon, in some boys, the testis preferentially stays higher exposing them to high temperature. These patients need to be carefully selected for surgery.
Key Points:
- Undescended Testis is found in 3% of term boys and 30% of preterm boys.
- When the testis does not come down by it self by 6 months, it is essential to consult a Paediatric Urologist with a view to correct.
- When left uncorrected, complications like infertility and torsion can result.
Hydronephrosis (PUJ)
This section discusses about blockage caused by PUJ obstruction. In this condition there is a blockage of urine at the junction of kidney and the pipe draining (ureter) – pelvi ureteric junction (PUJ). Because of this the kidney stretches. Often it affects one side alone although it can involve both kidneys.
- What are the symptoms of hydronephrosis?
- How is hydronephrosis diagnosed?
- How can hydronephrosis be treated?
- What does a pyeloplasty involve?
- What is the outlook for children with hydronephrosis?
What are the symptoms of hydronephrosis?
- Detected before birth (Antenatal Scans): The condition should not cause the mother to have any symptoms. Hydronephrosis should not cause the baby to have any problems before birth, but he or she needs close monitoring after birth to keep an eye on the condition.
- Colic or Pain abdomen: This can be a feature in older children. This is because of the urine in the kidney trying to push and overcome the blockage.
- Urinary Infection (UTI): Whenever there is any blockage to urine flow, the system can easily catch infection. These children may have fever, frequent painful urination etc.
How is hydronephrosis diagnosed?
- Ultrasound Scan: THydronephrosis is diagnosed using an ultrasound scan. It helps to determine the severity of blockage; reflected by the amount of dilatation.
- Nuclear Scan: For this test a small dose of medicine is injected in to the vein; pictures are taken with a gamma camera (like x-ray) every few minutes; this shows how fast the kidneys take up the medicine and how fast it leaves the kidney. When there is a blockage, the medicine stays in kidney for a long time. When the kidney function is poor; very little medicine is taken up by the kidney.
- MCU: This is mainly to exclude problems like reflux or a valve.
How can hydronephrosis be treated?
- If the hydronephrosis is diagnosed during pregnancy, early treatment will consist of monitoring with ultrasound, to check that the baby is growing normally and the kidneys are not getting too large. The baby will usually be born by a routine delivery.
- After the baby is born, the hydronephrosis will be monitored using ultrasound scans and Nuclear scans.
- When the hydronephrosis is getting worse or the kidney function is reducing surgery called pyeloplasty is recommended.
What does a pyeloplasty involve?
Under general anaesthesia, a small cut is made in the kidney region. The blocked portion is removed and reconnected. A small tube called stent may be kept to protect the sutures. It may be kept fully inside (needs removal under a second anaesthesia) or partly out (bedside removal after 7 days). The hospital stay is between 4-8 days. Children recover very well and it is not very painful as medicines will be given to take care of it. They can have normal feeds within 24 hours of operation.
What is the outlook for children with hydronephrosis?
- If the cause of the hydronephrosis is an obstruction and this is removed shortly after birth, kidneys will be able to work properly.
- The earlier the hydronephrosis is discovered, the better the outcome
Hydronephrosis & Antenatal Counselling
Currently most pregnant women undergo one or two ultrasound scans during their pregnancy. When the fetus is scanned, kidneys and the urinary tracts are analyzed, In addition the volume of liquor (amniotic fluid) also helps to suspect kidney problems. Of late stretching of the kidney (Hydronephrosis) is detected very frequently.
- Kidney Stretching (Hydronephrosis)
- Single Kidney Stretching (Unilateral Hydronephrosis)
- Both Kidneys Stretching (Bilateral Hydronephrosis)
- Consultation before birth (Antenatal Counseling)
Kidney Stretching (Hydronephrosis)
During scanning of 100-200 pregnant ladies, one fetus is found to have this abnormality. This usually happens because of a blockage in the urinary tract. Before proceeding further it is essential to describe the normal arrangement of the kidneys.
In human body there are two kidneys, one on either side of belly. From each kidney urine drains out via a tube called ‘ureter’ into a common urinary bladder. The bladder is located in the lower most part of belly. Once enough urine accumulates, it empties via a tube called ‘urethra’. Whenever there is a block in any of these tubes, kidney stretching results.
Single Kidney Stretching (Unilateral Hydron)
When only one kidney (right or left) stretches, blockage is suspected only on that side. When kidneys only stretch, the blockage is suspected at a higher location (PUJ obstruction). When the pipe draining the kidney also stretches, blockage is suspected at a lower location (VUJ obstruction).
Newborns with this problem need to be scanned on the third day after birth. In general very mild stretching is likely to settle spontaneously. Huge stretching requires surgery urgently to prevent loss of kidney function (renal failure). Children with moderate stretching need close monitoring with repeat scans and further tests. It is essential to consult a pediatric urologist to determine what tests are required and when a surgery could be avoided. Also it is essential to prevent urinary infection by taking a small dose of antibiotic once at night.
Both Kidneys Stretching (Bilateral Hydronephrosis)
When both kidneys stretch, they can be blocked separately. But usually they are blocked as urine exits the bladder in the ‘urethra’. In boys a valve like blockage can result in stretching of both kidneys (posterior urethral vale – PUV). Immediate endoscopic intervention after birth is essential to prevent urine infection and kidney failure.
Consultation before birth (Antenatal Counseling)
When there is a fetal kidney problem, there could be a lot of anxiety among parents. Consulting a paediatric urologist can relieve the anxieties and also provide answer to many questions. It will help to plan the type of delivery, place of delivery (where the treatment is available to the baby after birth), the type of tests required after birth. Also it helps to find out more about what is expected in the long run (prognosis) and whether the problem can occur again in future children (familial incidence).
Key Points:
- It is possible to determine kidney problems in the baby before birth.
- Most of the kidney problems correct spontaneously, although it is essential to confirm this by consulting a Paediatric Urologist
- A small proportion of babies require corrective surgery after birth.
- By consulting before delivery, parents can relieve their anxieties.
Intersex
The first question asked by grandparents after a baby is born is ‘is it a boy or girl’. This is often determined by looking at the genitalia. Intersex is a condition where the sex of the child could not be determined looking at the genitalia.
- What are the causes of intersex?
- How to deal with this at birth?
- Can the appearance be improved by an operation?
What are the causes of intersex?
The causes of intersex are many however it can be simplified as follows
- A Hypervirilised Girl: chromosome is XX but genitals are masculanised due to exposure to male hormones
- Undervirilised Boy: Chromosome is XY but the genitals are not well masculanised due to deficiency or failure of action of male hormones
- Mixture of problems: This can be at various levels; both XX and XY chromosomes or both testicular and ovarian tissues or multiple patterns
How to deal with this at birth?
It is essential to do the tests like chromosomes and harmonal tests soon after the birth to identify the problem. It is also essential not to name or fix gender for the baby before diagnosis. Once the problem is assessed doctors and parents should sit together and decide what is the best sex of rearing for the baby. If the sex is assigned by appearances without proper testing, it becomes socially very difficult to change gender once the child becomes old.
Hypospadias
Little baby boys pass urine like a fountain. Small lads can stand and pass urine straight with an ability to point the stream where they want, like a fire-man’s hose. This is possible because the urine comes out of the opening at the tip of the penis.
In boys with hypospadias, the opening is located on the under surface of penis. Because of this the urine is deviated downwards towards their feet. The picture shows normal arrangement and hypospadias.
- How is hypospadias detected?
- What are the consequences of Hypospadias?
- Do they have other birth defects? Can the same problem recur in future children?
- What is the right time to correct hypospadias?
- What are the chances of fertility after operation?
How is hypospadias detected?
Hypospadias occurs in one in 300 male newborns. When the paediatrician checks out the baby, or when the parents bath the baby, the following features can make one suspect hypospadias
- Urine opening on the under surface of the penis
- Penis being slightly bent downwards
- Excess foreskin on the top of the penis
What are the consequences of Hypospadias?
When hypospadias is left uncorrected, the following consequences can develop.
- Unlike the normal lads who can stand and pass urine, hypospadiac lads have to sit; if they stand and pass urine, it goes down the leg.
- When they get older, because of the bent in penis, sexual activities become difficult. Also they have much lower chance to have children, as they can’t deposit the sperm normally. The sperm leaks out through the opening located underneath.
- Sometimes the urinary opening is also small, leading to blockage in urine stream. This leaves them at a risk of urinary infection.
Do they have other birth defects? Can the same problem recur in future children?
In general, hypospadiac children do not have other kidney abnormalities. However in 10% of these kids, the testis may not be descended normally. When both testes have not come down normally, they can have associated hormone defects. When the first child or the father has hypospadias, there is a slightly higher chance (7-10%) for the future boys in the family to have the same birth defect.
What is the right time to correct hypospadias?
From 6 months onwards, hypospadias can be corrected by an operation. By completing the operation before 2-3 years of age, these children can be toilet trained normally like any other child. Not having an appearance like other boys at school, can lead to emotional problems in these children.
What are the chances of fertility after operation?
Most of the hypospadias belong to the mild variety and can be operated by a single stage operation. When the opening is too far down from the tip, they might require two-stage operation. The operation is usually done under general anesthesia and a catheter/ dressing is left for 5-7 days.
Three things are corrected during the operation.
- The opening is brought to the tip
- The penis is straightened
- Excess foreskin is removed (circumcision).
Optical magnification (microscope) and fine suture materials are essential for a successful result. When extra care is taken there is a very good (95%) success rate. In 5% the following complications can occur.
- The new opening gets small gradually (meatal stenosis)
- Urine leaks at the original site (Fistula)
Both these can be corrected by another minor operation; so the parents need not have undue concern about this.
Key Points:
- In children with hypospadias, the opening is on the under surface of penis.
- Because of this, these lads can’t stand and pass urine like normal children.
- They can have infertility in later life, if left uncorrected.
- By performing a corrective surgery at the right age, these can be avoided.
Phimosis / Circumcision
The term ‘Phimosis’ derived from Greek word for ‘muzzling’ has been widely applied to narrow foreskin. It is essential to understand normal appearance in a newborn child to know when Phimosis is abnormal or when it will require surgery
- What is a normal foreskin?
- Is it normal to have a non-retractile foreskin?
- Is it advisable to practice retraction to make it better?
- When is Phimosis a true problem?
- What is Circumcision?
- What does a circumcision involve? Are there any complications?
- Are there any alternatives to circumcision?
What is a normal foreskin?
The skin over the tip of penis normally folds on itself as a sleeve and attaches to the head of penis. This extra skin is called foreskin. In newborn babies the under surface of the foreskin is fused to the head of penis. Because of this in 95% of newborn babies the foreskin can not be pulled back. This is referred to as ‘physiological phimosis’ or ‘non retractile foreskin’. However as they gets older it separates slowly; upto 1-2 years of age, 50% of boys have a foreskin that can be pulled back; and by 15 years almost 90% have normal adult pattern.
Is it normal to have a non-retractile foreskin?
Up to 1-2 years of age there is a variable proportion of foreskin adherence to the penis. Sometimes there can be accumulation of white discharge called ‘smegma’ giving the appearance of ‘white pearls’ under the skin. Some times the foreskin balloons as the boy passes urine but there is no other problem. These are entirely with in the normal limit and should not be a cause of concern.
Is it advisable to practice retraction to make it better?
If parents resort to the practice of retraction exercises, they might overdo and can cause soreness and bleeding. Also excessive retraction with damage heals with scarring leading to real phimosis. Boys older than 7 years of age can attempt self retraction at bath. However it is essential to put it back after retraction, as skin left retracted can result in swelling called ‘paraphimosis’.
When is Phimosis a true problem?
- Scarring of the skin at the tip
- Recurrent infections
- Straining and only dribbling when passing urine
- Para phimosis (swelling and inability to put back the pulled foreskin)
What is Circumcision?
Circumcision is one of the oldest operations known to mankind. It basically involves removing the excess skin at the tip of the penis. There are several reasons for doing circumcision
- As a treatment: in true Phimosis
- As a preventive step: In children with recurrent urine infections (circumcision reduces the risk of cancer penis, sexually transmitted disease)
- For religious reasons: in Muslims and Jews
- Social reasons: ‘to look like Daddy!’; ‘to look like brother’
- As a routine: in some countries circumcision is performed routinely
What does a circumcision involve? Are there any complications?
Circumcision in children is usually done under general anesthesia, as a day case procedure. The operation lasts for around 30 minutes. The stitches are dissolvable and need not require removal. There can be a variable degree of swelling and the penis may look ugly for 2 weeks. As the head of penis has not been exposed, it undergoes drying and scabbing over it. Bleeding is a rare complication and usually settles spontaneously. The urinary opening on the penis can become narrow, especially if there is a skin problem called BXO. If this develops, it might require dilatation under general anesthesia.
Are there any alternatives to circumcision?
In an operation called ‘prepucioplasty’ the narrow ring of skin is divided across and sutured along. This widens the narrowing without removing the foreskin. For this operation to be successful, the boys need to self retract after the operation for 2-3 months
Key Points
- Non-retractile foreskin can be a normal developmental process in boys under 1 years of age.
- Circumcision is indicated if there are recurrent infections, or if there is narrowing with scarring.
- Circumcision is a safe operation that can be performed with out the need for over-night stay.
- For a good cosmetic result, and minimal complications, it has to be performed by a well trained surgeon
Emergencies
Torsion Testis
<
The testis can go for a twist inside the sac it is held. This results in loss of blood supply. If left untreated for more than 6 hours the testis loses function. Typical presentation is a 14 year old boy who develops severe pain, red ness and swelling of the sac of testis suddenly. It is very tender to touch. It is necessary to do a surgery immediately. There is no point in wasting crucial time on different tests. Surgery is diagnostic and also curative; if blood supply returns after untwisting the testis is preserved. If the blood supply is lost the testis may have to be removed. In either case opposite testis has to be fixed to prevent twisting on that side.

Kidney Injury
Children can sustain injury to kidney when there is blow to the loin either during a road traffic accident or a handle bar injury during cycling. The damage to the kidney can very from mild to serious type. There may be pain, blood in urine etc. CT scan is often required to confirm the extent of damage. Often the treatment is bed rest. Surgery is required only if there is continuous blood loss.
Urethral Injury
When boys fall on to a branch of a tree while climbing, or on cycle bar during cycling, the urethra located in between the legs is injured. When there is severe injury there will be blood from the tip of the penis and the child might not be able to pass urine; with urine accumulating in the bladder. A temporary diversion of urine directly from the belly may be required
.
Pyonephrosis
This term refers to pus in the kidney. This can be a result of obstruction to the urine flow and infection developing in it. It is a very serious problem requiring admission, IV fluids and IV antibiotics. In addition prompt relief of pressure has to be done to prevent complete loss of function in that kidney. The conditions that can lead to this include
- Blockage at the upper end of ureter (PUJ obstruction)
- Blockage at the lower end of ureter (VUJ obstruction)
Renal failure
If both kidneys are blocked then it can rapidly lead to renal failure. There can be very low to absent urine output (anuria). The conditions that can lead to this serious problem, even in the newborn period, include
- Posterior Urethral Valves
- Ureterocele blocking bladder outlet
They need to be carefully treated by experts in the field. Some times a simple catheter can revert the situation. Dialysis may be required before planning definitive surgery. Both of these problems can be tackled by a simple endoscopic surgery, relieving the blockage.
Appendicitis
What is Appendicitis?
In this condition there is infection followed by inflammation of the appendix. Appendix is a tail like structure found at the junction of small and large bowel. It is a rudimentary organ (not necessary for normal function of gut), only useful in animals.
What are the symptoms?
Typically there is pain in the right lower part of tummy. This is sudden onset with sometimes vomiting and fever associated. Any movement or cough will aggravate the pain. The pain to start of is in the centre of tummy, but with time localises to right lower part where the appendix is situated.
How is it diagnosed?
Often the diagnosis is by clinical examination. Typical location of pain is there. On pressing the right lower part, the child winces in pain. Blood counts may show elevated white cells. Ultrasound is often performed, not to look for appendix, but to exclude other causes of abdominal pain like kidney stones or ovarian cyst.
What is the treatment?
The treatment is emergency surgery to remove the infected appendix. Laparoscopic operation can be performed to minimise scar and hasten recovery.
What is the outcome?
If not operated in time, rupture of appendix can lead to a life threatening complication called peritonitis, where pus is spread all inside the abdomen. Operation and recovery after peritonitis are complicated. However for simple appendicitis, a quick recovery is the norm.
Paediatric Laparoscopic Surgery (Key Hole Surgery)
- What is a laparoscope? What is key-hole surgery?
- What are the advantages?
- Is it safe in children?
- What problems can be treated with laparoscopic surgery?
What is a laparoscope? What is key-hole surgery?
Laparoscope is a telescope like instrument to visualise organs inside. In key hole surgery there is no cut made; but surgery is performed through camera and instruments inserted via tiny holes.
What are the advantages?
- As there is no cut, there is no big scar
- The pain is almost nil as there is no cut
- The healing is fast
- Complications of wound healing are much less
- Children recover quicker and can be discharged quicker
- This helps to reduce the cost
- As they recover quicker can return to school quicker
Is it safe in children?
Laparoscopic surgery has been performed safely in children. There are no disadvantages. However one has to be prepared for open surgery in case there is instrument failure or technical difficulty.
What problems can be treated with laparoscopic surgery?
- Appendicitis
- Gall stones; spleen surgery
- Kidney surgery
- Varicocele
- Undescended testis
- Empyema (pus in chest)
- Ovarian problems
Incontinence, Neuropathic Bladder
What is urinary incontinence?
The term ‘Incontinence’ means lack of control. Urinary incontinence refers to the leakage of urine with no control over it. A large proportion of children who suffer from bed wetting or day time wetting do not have any major medical problem. They belong to a group called ‘Bladder Dysfunction’ which settles in course of time by itself or with the help of some medication. In children born with birth defects of the spine the incontinence is constant and can be a considerable problem. This is referred to as ‘Neuropathic Bladder’ or ‘Neurogenic Bladder’
What are the causes of neuropathic bladder?
In the condition called ‘Meningocele’ the spine is not closed fully and the baby is born with open spinal cord or a swelling in the back. These children undergo a neurosurgical correction at birth and present later with urinary incontinence by 4-5 years of age. In some children the back is normal to look but the spinal abnormality is hidden. Only on evaluation with further test like MRI scan a defect like spina bifida or tethered cord is detected. Spine injuries or injury to the nerves during an operation on the bowel within pelvis [‘pull through’ operation] also can cause damage to the bladder nerve supply.
What are the features of neuropathic bladder?
These children suffer from constant dribbling of urine and very severe leakage of urine. They may suffer from recurrent urinary infection. The may also have very poor control of bowel. This may be in the form of constipation or severe soiling of liquid stools. Some of them might also have associated problems like leg spasticity or deformity.
What are the risks faced by these children?
The nerve supply of the bladder and muscles that control urine are affected. The storage capacity as well as emptying capacity is impaired because of this. Stagnation of urine can predispose to recurrent urine infection. The bladder muscle generates high pressures during filling or emptying. The urine might go upstream towards the kidneys (reflux). The pressure and recurrent infections might damage the kidney and cause kidney failure.
What are the tests required?
Initial assessment of these children begins with an ultrasound scan to see whether the kidneys are affected and whether the bladder empties fully. A test called MCU identifies the shape of bladder and the presence of reflux. A more detailed assessment of bladder pressure and storage capacity can be done with a test called urodynamics. In this a computer records the bladder pressure during filling with saline.
What are the treatments available?
If the bladder pressures are high, a medicine is prescribed to relax the bladder. Constipation if present has to be treated effectively with medicine or enemas. When emptying of urine is a problem, these children need to use a small tube (catheter; pronounced ka- thee- ter) to empty the bladder. This procedure called ‘clean intermittent catheterisation’ is essentially passing the tiny tube via naturalis to empty the bladder using clean hands. Initially the parents may have to do this and once older the children learn how to do it. The very idea of passing a tube down the penis is worrying to the parents, however, worldwide a large proportion of children and adults have learnt this procedure and have prevented kidney failure and transplantation successfully. Initially there might be some reluctance, but once learnt this can be easily done as a routine. Often people worry about introducing infection as they pass tubes. In fact more people are saved from urine infection by regular emptying of bladder with a catheter.
When is surgery required?
Sometimes the bladder is too small and does not store enough urine. It may also generate high pressure and can cause kidney damage. In such a situation, the bladder is enlarged by an operation using a piece of bowel. This procedure called bladder augmentation increases the bladder capacity and reduces the pressure. Once this procedure is done, the bladder needs to be regularly emptied with catheterization. If catheterization via natural route is not possible because of pain or some other defect, they need a surgery called ‘Mitrofanoff’. In this procedure the appendix is used to create a tunnel between the belly and bladder. Through this a tube can be passed more easily without pain to empty the bladder.
Key Points
- Constant leakage of urine and a bad urine odour can affect the child’s self image if left untreated.
- In modern medicine childhood urinary incontinence can be effectively treated.
- Prompt treatment can prevent multiple urine infections as well as kidney failure.
Bedwetting
Bedwetting (nocturnal enuresis) is involuntary voiding of urine during sleep at least three times a week in a child aged 5 years or older. It is a common worldwide problem affecting both boys and girls below 16 years. It can be a distressing experience for the child and may lead to loss of self-esteem and isolation. Children fear being discovered and are afraid to go to relatives’ or friends’ house. Although most parents are supportive, up to 30% parents become intolerant towards their child.
- How common is bedwetting? Can it correct itself?
- Why does bedwetting happen? Is it anyone’s fault?
- Is it caused by any underlying problem?
- What treatment is available? Can any dietary modification help?
- Do’s
- Don’ts
How common is bedwetting? Can it correct itself?
At 5 years of age, around 1 in 6 children still wet the bed. This means that in a school class of thirty there will be five who wet the bed regularly. Because the children and their parents are too embarrassed to talk about the problem it is unlikely that they will be known to each other. Most of these children spontaneously grow out of it. By the age of 10 only one in 15 still wet the bed. Even in adulthood 1 in 100 still suffers from the problem.
Why does bedwetting happen? Is it anyone’s fault?
It is important to remember that it is not the child’s fault. Parents must also not blame themselves. Getting angry or punishing the child could make the problem worse. Supporting and praising the efforts of the child to stay dry will help the child to become dry sooner. Getting medical help relieves the anguish for the family.
The cause of bedwetting is usually a combination of three factors.
- Over production of urine at night
- Hyperactivity of the bladder
- Lack of arousal from sleep
Stressful early life events can trigger bedwetting in those who have previously been dry for a long period.
Is it caused by any underlying problem?
Children with isolated bedwetting usually do not have any underlying problem. However if a child has been wet right from birth, always wet day and night, or never achieved toilet training, then it is essential to see a Paediatric Urologist to make sure that there is no associated medical problem like ectopic ureter, where one kidney drains not into the bladder but, outside the body directly.
What treatment is available? Can any dietary modification help?
Often simple methods like waking up the child (alarms) and giving awards for a dry night (star chart) are undertaken. If bladder over activity is suspected, a bladder relaxing medication is prescribed. If night time alone is a problem, a medicine to reduce the volume of urine in the night is prescribed. When urine infection is suspected, an antibiotic is prescribed.
It is essential to avoid bladder irritants as black current, coffee or coke. Constipation can make bladder problems worse. Taking plenty of fruits and vegetables can help to prevent this. Often parents restrict children’s water intake. This is not necessary; in fact these children need plenty of water and regular toilet visits during the day.
Do’s
- Stay calm, be prepared and try not to worry
- Encourage your child for staying dry; give awards for dry nights
- Encourage the child to drink plenty; it is important that they recognize the feeling of full bladder
- Avoid fizzy drinks, tea, coffee, chocolate; these can irritate bladder and can cause more urine production
- Ensure that the child goes to toilet before bed
- Make sure that easy access to toilet is available at night
- Allow the child to help with changing the bed; this helps them to understand the problem and overcome it.
- Make sure that the child has a bath each morning. This removes the smell of urine and avoids the child being teased at school.
Don’ts
- Do not get cross with your child; it is not their fault
- Do not use waking the child as a long term strategy to overcome bedwetting; instead get help from a doctor.
- Don’t give up. 99% of these children get better by adulthood.
Kidney Stones in Children
There is a wide misconception that only adults develop stones. On the contrary kidney stones are very common in children living in hot climates.
- How is a stone formed in urine?
- What are the symptoms of urine stones?
- How is a stone detected?
- What are the treatments available to remove the stones?
- What is Endoscopic treatment?
- What is Breaking Stones?
- Can stones come back? How can we prevent this?
- What are the dietary restrictions in children with stones?
How is a stone formed in urine?
Urine is basically made of unwanted salts in the body. Presence of a reasonable amount of water is essential to prevent stone formation. When the the water content is less, the urine becomes concentrated and favours stone formation. Also stagnation to urine flow promotes stone formation. Some children with stones have birth defects that make them pass more calcium and less citrate in urine. Children with recurrent urine infection are more prone to develop stones; stone in turn promotes urine infection.
What are the symptoms of urine stones?
- There can be no symptoms when a stone is present.
- When a stone is blocking urine passage in the kidney or urinary tubes, severe loin pain results.
- When there is a stone in the urinary bladder, there will be pain at lower part of belly or the penis.
- Pain when passing urine, blood in urine or even passing small stones or gravel can be present.
- Small babies cant tell these. When children cry while passing urine or when there is urine infection, it is essential to rule out a stone.
How is a stone detected?
When children experience the above symptoms, urine is tested in the lab. Presence of excess red cells or white cells; and presence of crystals in the urine suggests urinary stone disease. Ultrasound scan helps to find out whether there is a stone, the position, size and number of stones. In addition special tests like IVP, X-Ray, or CT scan may be required.
What are the treatments available to remove the stones?
There is a general misconception that childhood stones always require open surgery. Like adults children also can be treated without open surgery. In modern medicine facilities are available to break stones and 80% are removed without open surgery. For this it is essential to consult a pediatric urologist trained in this field.
What is Endoscopic treatment?
When stone is present in the bladder, it can be removed with the help of an endoscope. Endoscope is a small tube with a camera that is passed up via the urinary passage. The stones are grasped with small grabbers. Bigger stones can be broken with the help of a technique called lithotripsy. As children won’t stay still, they need a general anesthesia. To prevent blockage by broken stone pieces, a small tube called stent is left in for 2-3 weeks.
What is Breaking Stones?
A technique called ESWL uses sound waves to break stone. With the help of an x-ray or a scan the stone is focused. ESWL machine breaks the stone in less than an hour. Sometimes a second sitting may be required for complete stone clearance. With this treatment, children can return home with a couple of days. Small children need general anesthesia, as they have to lay still for this.
Can stones come back? How can we prevent this?
Children have a 20-50% higher chance for the stone recurrence. Problems like passing excess calcium in urine can be there. It is essential to identify this to prevent further stone formation. Regular toileting and drinking plenty of water are essential to prevent stones and urine infection.
What are the dietary restrictions in children with stones?
- In general drinking plenty of water (10-20 cups) helps to reduce stone formation.
- Salt should be restricted in diet.
- Non vegetarian foods and milk products need to be reduced.
- Cabbage, spinach, cashew, walnut etc need to be avoided.
- Coffee, tea, cola, apple and grape juices need to be restricted.
- Orange and lime juices are good.
- Vitamin D and calcium tonics should be avoided.
Key Points
- Like adults children can also develop urinary stones.
- Children can have underlying medical problems that make them prone to develop stones.
- It is essential to identify and treat these to prevent stone recurrence.
- With the advent of newer facilities, 80% of stones in children can be removed without open surgery.
- It is essential to consult a paediatric urologist trained in this area to obtain the appropriate treatment.
Urinary infection/Vesico Ureteric Reflux
A child is considered to have urinary tract infection (UTI) when the urine of the child grows bacteria during a microbiological test and the amount is significantly high (more than one lakh per ml). During childhood 5% of girls and 2% of boys get UTI. In the new-born period more boys get UTI than girls. Among the girls half can get a second UTI within a year.
- Why is UTI important in children?
- How do we suspect urinary infection?
- How is UTI diagnosed?
- How is UTI managed?
- What is Vesico Ureteric Reflux (VUR)?
- How do we diagnose VUR?
- Can it be familial?
- What is the treatment for VUR?
- Is it safe to give a child long term antibiotics? Will it reduce the immunity?
- When is operation required for VUR? What does it involve?
- What are the other problems that might require operation?
- What are the general measures one should take to prevent urine infections?
Why is UTI important in children?
The incidence of underlying kidney problem is far higher in children compared to adults. 30-50% of children with UTI can have a kidney problem. If left untreated, they can lead to multiple infection, kidney scarring and in the long term hypertension and renal failure.
How do we suspect urinary infection?
When the UTI involves bladder alone, one experiences frequency, pain and burning sensation while passing urine. When the kidneys are also affected, high fever, vomiting, tummy pain and feeling unwell, can be the features.
How is UTI diagnosed?
Initial urine tests with microscope can help to identify presence of UTI. However it is confirmed only after growing organisms in a large number when tested in micro lab.
How is UTI managed?
After confirming the diagnosis, it is usually treated with a course of oral antibiotics. If kidney infection is suspected, the child may require hospitalization for IV fluids and antibiotics via IV route. Once UTI is treated, an ultrasound scan is requested to look for any underlying abnormalities.
What is Vesico Ureteric Reflux (VUR)?
In normal state, the urine travels in a one-way direction from kidneys to the bladder via the ureter. Once in bladder, the urine does not go back up either during storage or emptying. But in children with Vesico Ureteric Reflux (VUR), the urine goes upstream towards the kidneys. Because of this the kidneys are exposed to serious infection and scarring during any urinary infection.
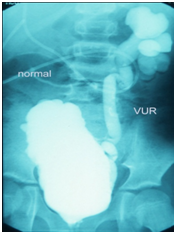
How do we diagnose VUR?
A test called MCU is done to diagnose VUR. In this a special radio opaque dye is injected via a catheter into the bladder. X-rays are taken while the child passes urine. Normally urine should not go up towards kidneys. But in children with VUR it goes up.
Can it be familial?
There is a slightly higher chance in future kids to have VUR when there is a kid with this problem in the family.
What is the treatment for VUR?
When VUR is present the usual treatment is to put them on long term low dose antibiotics (sometimes up to 4-5 years). This prevents the kidney getting infected. Most of them do not require surgery.
Is it safe to give a child long term antibiotics? Will it reduce the immunity?<
Long term antibiotics are only to protect kidneys. They are found to be safe and they do not cause reduction in immunity.
When is operation required for VUR? What does it involve?
When a child gets recurrent urine infections despite being on antibiotics, or when the reflux is very high grade with kidney scarring, then surgery is recommended. In this the length of ureter inside the bladder is increased, thereby creating a one-way valve. This prevents urine going back upstream. It is done under general anesthesia and involves 5-7 days hospital stay. The success rate is above 95%.
What are the other problems that might require operation?
In boys, circumcision has shown to reduce UTI significantly. If there is a blockage to the urinary tract, it will need correction. If urinary stones are present, they need to be removed. If there are congenital abnormalities of kidneys predisposing to UTI, they may need correction
What are the general measures one should take to prevent urine infections?
- Encourage your child to drink plenty of water
- Ask them to go to toilet regularly
- Prevent constipation by giving plenty of vegetables and fruits
- Avoid bladder irritants like coffee, tea and coke.
- Avoid exposing genitalia to soap, or shampoo, or bubble baths.
- Bio-yoghurts, curd etc have been shown to reduce UTI.
Key Points
- UTI in children need to be properly diagnosed and treated.
- Children are more likely to have underlying kidney abnormalities than adults.
- Some of them require surgery to prevent long term damage to the kidneys.
Posterior Urethral Valves (PUV)
Posterior urethral valves (PUV) is a condition found only in boys. PUV occurs in one in every 8000 boys born. It affects the urethra (the tube which runs from the bladder to the outside). In boys with PUV, the urethra has a blockage in it near the bladder. This makes it difficult for them to pass urine. As the bladder pushes hard to get the urine out, it causes pressure which may result in urine being pushed back from the bladder into the ureters and kidneys (reflux). This causes the kidneys and bladder to swell. This also may lead to kidney damage.
- What are the symptoms of PUV?
- How is it diagnosed?
- How can PUV be treated?
- What is the outlook for children with PUV?
What are the symptoms of PUV?
There are various symptoms associated with PUV, but they may not affect every child in the same way. The degree of blockage affects the severity of the symptoms. These boys can have
- Urinary tract infections (UTIs)
- Difficulty urinating
- A weak stream of urine
- Unusually frequent urination
- Bedwetting after toilet training has been successful
- Poor weight gain
- An enlarged bladder, so that it can be felt through the abdomen as a lump
How is it diagnosed?
PUV can be diagnosed by a routine ultrasound scan during pregnancy if the bladder, ureters or kidneys are swollen. It can also be diagnosed in a newborn baby if the bladder is swollen and urine dribbles constantly. If the blockage is not severe the condition can remain undetected until the child has symptoms as above.
- Ultrasound of abdomen – this is very similar to the ultrasound scan that most women have during pregnancy. It creates a picture of the organs inside the body and shows how well they are working.
- Micturiting cystourethrogram (MCU) – this test shows urine passing from the bladder to the urethra and then to the outside. It will also show if the urine is flowing backwards towards the ureters and kidneys (reflux).
- Blood tests – these will show how well your child’s kidneys are working and check that there is enough fluid inside the body.
Other tests and scans may be needed to check that other parts of the urinary system are working properly. These can include kidney and bladder function tests.
How can PUV be treated?
There are several options for treatment, depending on how severely the symptoms are affecting your child:
- The first course of action usually deals with the symptoms and includes putting a catheter (thin, plastic tube) into the bladder to drain away the urine. Any UTIs and fluid imbalance will also be treated with antibiotics and intravenous (IV) fluids, which are delivered directly into a vein.
- Following this the valves are destroyed with the help of a cystoscope (a tube with a light on the end) – called Cystoscopic fulgration. This is a delicate procedure and needs to be done under general anaesthesia. Following this a catheter is left in for a few days. Some times a second sitting is required after a few months.
What is the outlook for children with PUV?
The outlook depends on how much damage has already occurred in the kidneys. Your doctors will be able to give you a better idea once they have all of your son’s test and blood results. It is essential to keep up with the follow up appointments as they need long term monitoring; some time for years together.


